What is Harm Reduction?
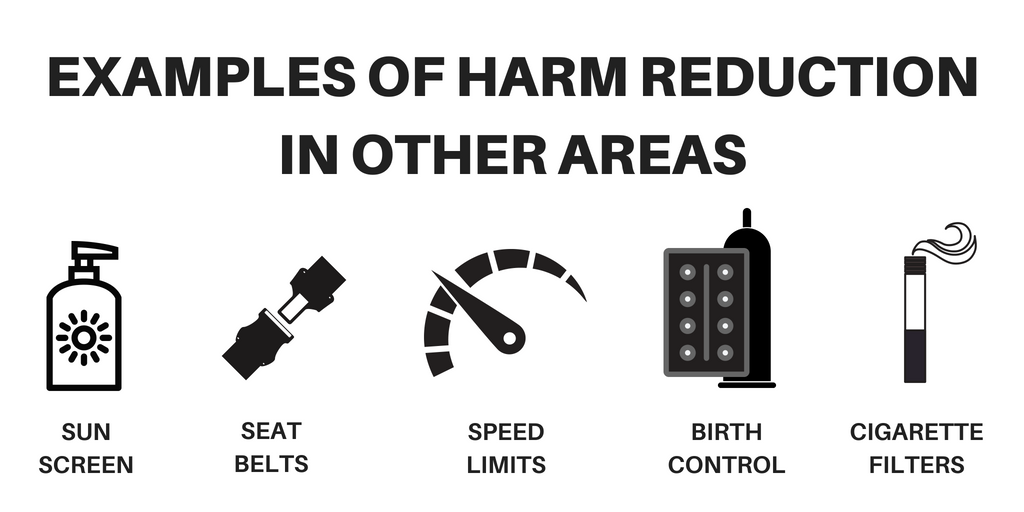
Harm reduction “is an evidence-based approach that is critical to engaging with people who use drugs and equipping them with life-saving tools and information to create positive change in their lives and potentially save their lives” (SAMHSA). It can also be defined as a set of practical strategies and ideas aimed at reducing negative consequences associated with drug and alcohol use.
- Helmets – prevent us from getting potentially life threatening head injuries while riding a bicycle
- Designated drivers – helps keep a group safe while driving sober
- Crisis/mental health support lines – ready to help assist anyone when in need
- And more
What is Narcan?
Narcan, a brand name for Naloxone, is a safe medication that can reverse an opioid overdose. It is important to understand that Naloxone isn’t meant to encourage teens to continue to consume prescription drugs, but it is there to prevent death. It is safe to use:
- When someone is experiencing opioid overdose-like symptoms
- On all ages, when pregnant people
Note that even if the person you believe may be experiencing an overdose is actually not overdosing, Naloxone is still safe to administer and can be given through a nasal spray, an injection, or an IV. It is non addictive and there is no potential for abuse. It will only work if the person consumed opioids.
What is an Opioid?
According to Johns Hopkins, “opioids are a class of drugs that derive from, or mimic, natural substances found in the opium poppy plant.” Opioids can be used for medicinal purposes to treat things like:
- Post-surgical pain
- Severe pain due to trauma or disease
- Coughing
- Diarrhea
Opioids can also be consumed for a euphoric feeling. The want to have this feeling leads to addiction. Addiction has severe effects on mental health in teens like: depression, hopelessness, irritability/aggression, irresponsibility/poor judgment in decision-making, abrupt behavior changes (sleeping and eating patterns), poor performance in school, and more (McLean Hospital).
Some common prescription opioids are: hydrocodone, oxycodone, oxymorphone, morphine, codeine, and fentanyl (National Institute on Drug Abuse). Not all pain-relief medication are opioids, so the following are not opioids: Acetaminophen (Tylenol, Excedrin, Vanquish), Aspirin (Bayer, Bufferin, Ecotrin, Excedrin, Vanquish), Diclofenac (Voltaren Gel), Ibuprofen (Advil, Motrin IB), and Naproxen (Aleve) (Kansas Board of Pharmacy). Just because these are not opioids, does not mean that they will not have severe side effects when too much is consumed. All medication, including over the counter, should be treated with care.
Opioid Overdose Risks & Signs
The following increase chances of an overdose: decreased tolerance after a period of not using opioid, mixing opioids with other substances like alcohol, quality and consistency of the drugs, and using it alone. An overdose cannot happen through skin to skin contact or breathing in secondhand smoke. These are the signs of an overdose to look out for (CDPH):
- Small, constricted “pinpoint pupils”
- Falling asleep or losing consciousness
- Slow, weak, or no breathing
- Choking or gurgling sounds
- Unable to speak
- Limp body
- Cold and/or clammy skin
- Discolored skin (especially in lips and nails)
How do you administer Narcan?
- Get someone else in the room should immediately call 9-1-1 as soon as an opiod overdose is suspected. If you are by yourself, call 9-1-1 yourself.
- Attempt to see if the person is responsive. Shake them and shout for them to wake up. If there is no response, rub their chest bone with your knuckles for 5-10 seconds to check for further response. Tell them what you are doing and that you’re going to give them Narcan.
- Administer Narcan (read instructions provided if needed). Each box for the nasal spray consists of two separate doses.
- Place two fingers on either side of the nozzle and your thumb on the red plunger. Insert the tip of the nozzle into either nostril until your fingers are pressed against their nose.
- Tilt the person’s head back and provide support under the neck with your hand.
- Press the red plunger firmly to give the dose and remove it after administering it
- If the person is not breathing, give them rescue breaths and continue to do so until it is unnecessary. Watch the person’s breathing and responsiveness until help arrives.
- If there is no response in 3 minutes, administer a second dose of Narcan and continue rescue breathing
- Put the person into the recovery position (on their side and head supported) so if they person throws up, they will not choke.
Where to get it?
If you are local to Colorado near the Broomfield area, you can get Narcan for free at the Broomfield Library. This also applies to teens. You can also go to your local CVS Pharmacy and purchase OTC Narcan without a prescription. Check out your local guidelines and possible places where your state, city, and county may distribute Narcan.
Debunking 6 Popular Myths
These six facts were directly taken from Indian State Department of Health.
Myth #1: Naloxone encourages substance users to take drugs. Fact: Research has shown that naloxone does not lead to more drug use or riskier drug use. In fact, some studies have shown that naloxone results in a decreased use of opioids. Naloxone also causes opioid withdrawal symptoms, which is an effective abuse deterrent.
Myth #2: Naloxone prevents substance users from seeking treatment. Fact: There is no evidence to support that naloxone prevents substance users from entering a treatment program. In fact, the near death experience often serves as a catalyst to seeking treatment and maintaining recovery.
Myth #3: Naloxone makes people violent. Fact: Every medical and emergency service has an associated cost. Substance use disorder and overdose is a recognized health condition that deserves attention. In 2020, 91,799 drug overdose deaths occurred in the United States. Many of these deaths could have been prevented by naloxone.
Myth #4: Only doctors can prescribe naloxone. Fact: One of the most common side effects of naloxone administration in patients is confusion and disorientation. It is rare for someone to wake up from an overdose and become combative. This is especially rare if naloxone is administered by someone they know and trust.
Myth #5: Naloxone is taking too much of the public’s funds and attention. Fact: The Indiana State Health Commissioner issued a standing order in 2016 that allows anyone to go directly to a pharmacy and purchase naloxone without having to obtain a prescription from their doctor. The same is true for the state of Colorado. Check what your state, city and county laws are for the use and purchase of Naloxone.
Myth #6: First responders administer naloxone to the same people over and over again. Fact: Research has shown that naloxone does not lead to more drug use or riskier drug use. In fact, some studies have shown that naloxone results in a decreased use of opioids. Naloxone also causes opioid withdrawal symptoms, which is an effective abuse deterrent.
Additional Resources
If you are wanting hotlines, support groups and more, check out: Resources for Teens | Mental Health, Bullying, and More…